Many speech-language pathologists provide care to tracheostomy patients with speech and/or swallowing issues as evidenced by the references published 1,2,3. The American Speech and Hearing Association has acknowledged our participation by stating that the care of atypical communication and swallowing issues associated with such laryngeal anomalies as tracheostomy patients is within our scope of practice 4. Some entities, such as licensing boards and state associations, have discussed the extent to which the speech-language pathologist should be involved in the suctioning of trach patients and have published guidelines 5. These entities have also suggested that we review relevant scope of practice documents, position statements, and related ethics issues prior to the implementation of care 5,6 . There are, however, no competencies or recommendations regarding the knowledge or skills needed by speech-language pathologists specific to tracheostomy care including suctioning.
In an effort to determine the extent of care provided by speech pathologist to the tracheostomized patient, a survey was posted via the voice list server hosted by Dr. Karnell at University of Iowa entitled, ”Management of Tracheostomized and Ventilator Dependent Patients.” The results indicated that care of the tracheostomized patient extends not only to the evaluation of speech and swallowing issue, but to the assessment and care of the tracheostomy tube and tracheotomy site as well.
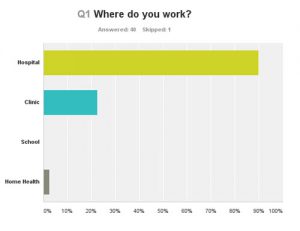
Of the 40 speech pathologists that responded to the survey, 90% of the respondents worked with tracheostomy patients, and of those working with tracheostomy patients, 90% worked in the hospital setting.
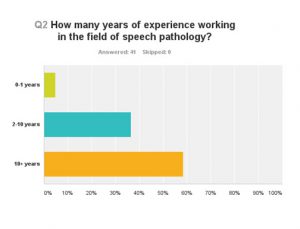
The majority of the respondents had greater than 10 years of experience in the field of speech pathology
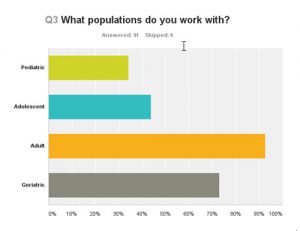
While most of the speech pathologists surveyed worked with adults, there was a surprising number of therapists working with the pediatric population and young adults.
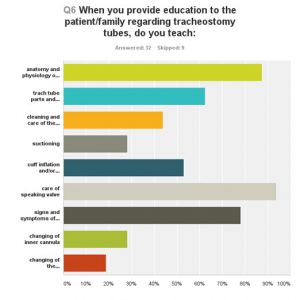
As expected, all of the speech pathologists surveyed not only assessed speech and swallowing, but also were involved in direct tracheostomy care including changing of the inner cannula and tracheostomy tube, deflating and inflating the cuff, suctioning, placing or removing the speaking valve, cleaning the trach site, changing the dressing, and making recommendations for down sizing of the tracheostomy tube to accommodate the PMSV.
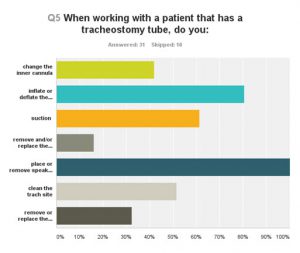
Speech pathologists were also involved in educating others in all aspects of tracheostomy care including but limited to changing the inner cannula, cuff inflation and deflation, removal and replacement of the entire tracheostomy tube, cleaning around the tracheostomy site, etc.
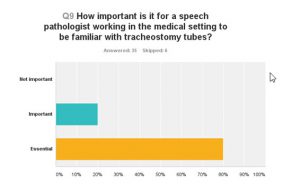
Most importantly, 80% of the respondents reported that it is essential that speech-language pathologists have the necessary knowledge and skills required to work with the tracheostomized patient when working in a medical setting.
Unfortunately, speech-language pathologists in the United States, as a profession, do not have a specific competency guideline or a list of required skills necessary to provide care to tracheostomy patients other than those developed by individual entities or work settings. The Speech Pathology Association of Australia recognized that the role of speech pathologists working with the tracheostomy patients and developed the Tracheostomy Management Position Paper in 2005 to address “…the role of the speech pathologist in the process of decannulation, management of paediatric patients and the management of ventilator assisted patients.”
Our association needs to move forward to develop a competency guideline to help its members with establishing a set of specific skills that define universally applicable characteristic of practice, which can then be used to assess clinical competency in this specialized area of practice.
References
1 Karen J. Dikeman and Marta S. Kazandjian, Communication and Swallowing Management of tracheostomized and ventilator-dependent adults 2nd Edition,(2003), Thomson Delmar Learning.
2 Mason, M. (Ed). (1993) Speech pathology for tracheostomized and ventilator dependent patients. Newport Beach, CA: Voicing!
3 Carrie Windhorst, MS, CCC-SLP; Ricque Harth, CCC-SLP; Cheryl Wagoner, CCC-SLP. Patients Requiring Tracheostomy and Mechanical Ventilation. A Model for Interdisciplinary Decision-Making. The ASHA Leader, January 2009, Vol. 14, 10-13.
4 American Speech-Language Hearing Association, (2004). Scope of practice in audiology. Available fromwww.asha.org/policy
5 http://dhmh.maryland.gov/boardsahs/professionals/SitePages/guidelines-tracheal-suctioning.aspx, (2013) SLP guidelines for use of tracheal suctioning.
